Abstract
BACKGROUND
Immune thrombocytopenia (ITP) is a disease characterized by low platelet count (less than 150,000 per microliter) caused by acquired autoantibodies against platelet antigens. It is one of the most common causes of thrombocytopenia in adults (Zainal et al., 2019).
The American Society of Hematology suggests inpatient management in patients presenting with severe or life-threatening bleeding, and those with newly diagnosed ITP and a platelet count less than 20,000 u/L who are asymptomatic or have minor bleeding (Neunert et al., 2019). However, there is limited information regarding the outcomes of adults hospitalized with ITP, and little research reflecting how hospitalization rates may have evolved over the years with the advent of new therapies such as monoclonal antibodies and thrombopoietin receptor agonists, and the decreasing rates of splenectomy.
This study evaluates the epidemiological trends and the influence of gender, race, and economic disparities in outcomes among hospitalized patients with ITP from 2010 to 2019.
METHODS
Using the National Inpatient Sample (NIS) database, we identified adult patients admitted for immune thrombocytopenia from 2010 to 2019 using ICD-9 and ICD-10 codes. Trends for in-hospital mortality, total hospital charges, and length of hospital stay, were evaluated for the entirety of the cohort and then analyzed separately for subgroups based on gender, race, and income quartile. Multivariate logistic regression analysis was conducted to adjust for confounders.
RESULTS
Hospital admissions for ITP remained stable from 2010 to 2019. Most patients were female (57.8%) and White (60%), followed by Hispanic (14.2%) and Black (12.7%) patients. There was a statistically significant increase in the proportion of patients with a Charlson score > 3 (p < 0.01), which reflects an overall increase in the comorbidity burden in the U.S. population.
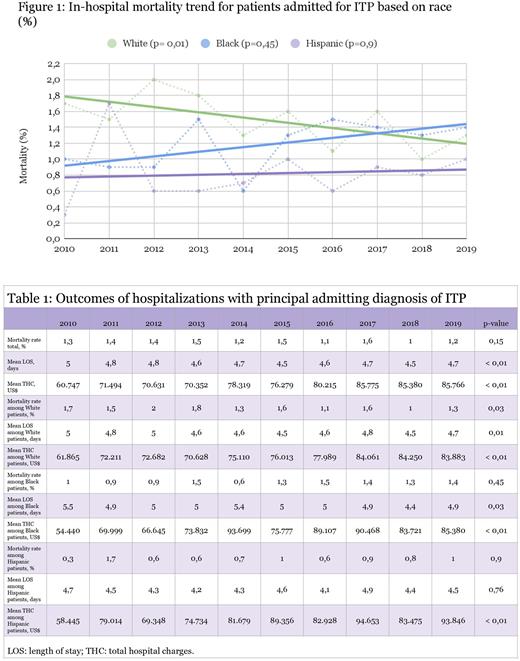
Overall, mortality remained stable at 1-1.6% (Table 1). However, there was a statistically significant decrease in mortality for White patients admitted with ITP (Figure 1), when adjusted for age and gender (p = 0.03). Meanwhile, there was an increase in mortality for Black patients, although this did not reach statistical significance. Outcomes did not differ significantly between males and females or between different income quartiles.
There was an increase in total charges when adjusted for inflation in all subgroups (p < 0.01). Length of stay decreased for the total population and most subgroups, with the exception of Hispanic patients and those at a higher income quartile, where this was not statistically significant.
CONCLUSION
Although advancements in treatment have been made in the management of ITP, this has not resulted in a decrease in the number of hospitalizations or total hospitalization charges, even though there was a small decrease in length of stay. Furthermore, a decrease in mortality was observed in White patients but not Black or Hispanic patients; this could potentially indicate disparities in access to care for these minorities. Prospective studies are needed to better understand and address inequalities in the care of patients with ITP as well as to further characterize the financial burden of the disease.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal